Laboratory Testing
Example 2: Rapid Strep Test I

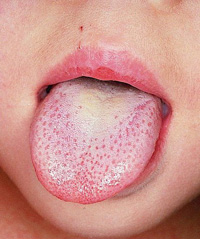
Let’s think about a situation where a school age child presents with sore throat, acute onset of fever (103º F), and one episode of vomiting during April. In early spring the prevalence of strep tonsillitis is higher than at other times of the year. There is also a recent outbreak of strep throat in the school. The physical exam is remarkable for tonsillar hypertrophy with exudate.
What diagnostic test should you consider?
Current sensitivity on the 35 CLIA-waved rapid strep test (RST) ranges from 62% to 95% (Blazek, 2008). Let’s say the sensitivity of the RST you are using is 77% and the current incidence of strep in your area is 25%, what else do you want to consider?
Consider cost of the test, age of the child, examiner’s technique in doing the test, and clinical presentation.
Based on the child’s presentation, your clinical suspicion of strep is high. The presence of multiple recent cases of strep throat also increases the prior likelihood of strep infection. How does the prevalence of a test affect the interpretation of a positive rapid strep test?
Slide the bar to see how changing the cutpoint alters the sensitivity and the specificity.
Number of patients
| = False Positives | |
| = True Positives | |
| = True Negatives | |
| = False Negatives |
Sensitivity = 0
Specificity = 0
The RST test costs $15.00, but an in-house culture costs $10.00. Given the presentation of the child, which test would be more cost effective?
What would happen if a 12 month old child presented with a sore throat, acute onset of fever (103º F) and one episode of vomiting in the summer instead of spring? How does this patient history affect the likelihood that a positive is a true positive?
Strep pharyngitis is less likely in the summer; therefore, there would be more false positives.
What about a negative result? The specificity of the 35 CLIA RST ranges from 85 to 100% (Blazek, 2008). There will always be false negatives. Strep throat is a self limited disease which we treat primarily to prevent rheumatic fever. In practice we treat all positives as true infection, prescribe antibiotics and do not send an in-house culture for confirmatory testing. As a result of false positives, people without disease are treated with antibiotics even in seasons when the prevalence of the disease is low. It is acceptable to treat patient with positive CLIA to allow earlier treatment. On the other hand, we do not accept false negatives. Our primary goal of therapy in strep pharyngitis is the prevention of rheumatic fever. Therefore, when the CLIA is negative, a confirmatory culture is ordered and if it is positive, the child is treated with antibiotics.
We need to make a compromise between too many false positives (FP) and too many false negatives (FN). What we choose will depend on the purpose of our test. In most situations we want a balance between false positives and false negatives. But sometimes we want to be sure we capture as close to 100% of people with the disease as possible so we are willing to accept some false positives in order to make sure we get all the people with disease.